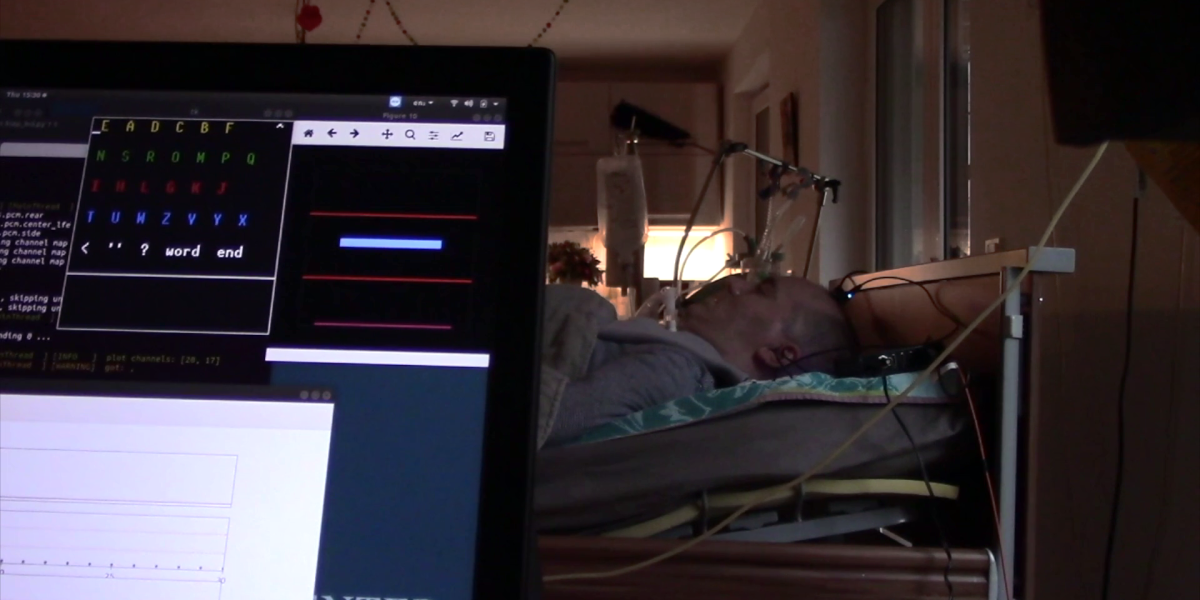
On meeting the man in February 2018, Chaudhary tried to automate the communication system that the family was already using. The team connected an eye-tracking device to computer software that would read out colors and row numbers, allowing the man to select letters one at a time using his eye movements to spell out words.
But as the man increasingly lost control over his eye movements, he became less able to communicate using that device, too. “We proposed implanting [an electrode],” says Chaudhary. Tiny electrodes can be implanted in the brain to record the electrical activity of brain cells directly. The procedure—which tends to involve drilling a hole in the skull and cutting away the brain’s protective layers—comes with a small risk of infection and damage to the brain. So it was a last resort, says Birbaumer. “If the [non-invasive] BCIs and the eye-trackers don’t work anymore, there is no other choice,” he says.
The man consented to the procedure using eye movements, says Chaudhary. His wife and sister also gave their consent. By the time the procedure had been approved by an ethics committee and Germany’s Federal Institute for Drugs and Medical Devices at the end of 2019, the man had lost the ability to use the eye-tracking device. In March 2019, surgeons implanted two tiny electrode grids, each measuring 1.5 millimeters across, into the man’s motor cortex—a region at the top of the brain responsible for controlling movement.
Turning signals into commands
The day after the electrode was implanted, the team began trying to help the man communicate. At first, the man was asked to imagine making physical movements—this has helped other recipients control prosthetic limbs and exoskeletons, and is the approach that Elon Musk’s company Neuralink plans to take. The idea is to get a reliable signal from the brain, and translate this into some kind of command.
But the team couldn’t get it to work. After 12 weeks of trying, they scrapped the idea and decided to try an approach called neurofeedback instead. Neurofeedback works by showing a person their brain activity in real time so that they can learn how to control it. In this case, when the electrodes in the man’s brain recorded an increase in activity, a computer would play a rising audio tone. A fall in brain activity would play a descending tone.
“Within two days, he was able to increase and decrease the frequency of a sound tone,” says Chaudhary, who says he visited the man in his home every weekday during 2019, until coronavirus hit. “It was just incredible.” The man eventually learned to control his brain activity so that he could play a rising tone to signal “yes” and a descending tone to signal “no.”
The team then introduced software that mimicked the paper-based computer system the man had originally used to communicate with his family. The man would hear the word “yellow” or “blue” for example, to choose a block of letters from which to select. He would then be played individual letters and use a rising or descending tone to either select or dismiss each (see video).
Effortless
In this way, the man was soon able to communicate entire sentences. “[His family] were so excited to hear what he had to say,” says Chaudhary, who, along with his colleagues, published their findings in the journal Nature Communications on Tuesday. One of the first sentences the man spelled was translated as “boys, it works so effortlessly.”
Communication was still slow—it takes around a minute to select each letter. But researchers believe the device has significantly improved the man’s quality of life. He has asked for specific meals and soups, directed carers on how to move and massage his legs, and asked to watch films with his young son, for example. One sentence translated as “I love my cool son.”
“Many times, I was with him until midnight, or past midnight,” says Chaudhary. “The last word was always ‘beer.’”
One of the first sentences the man spelled was translated as “boys, it works so effortlessly.”
Chaudhary envisions developing a catalog of frequently used words that could eventually allow software to autocomplete the man’s words as he spells them, for example. “There are many ways in which we could make it faster,” he says.
No one knows how long the electrodes will last in the man’s brain, but other studies have found that similar electrodes are still functioning five years after being implanted in other people. But for a locked-in person, “a single day can make a difference,” says Kianoush Nazarpour at the University of Edinburgh, who was not involved in the work. “That is a fundamental opportunity for them to regain choice and control of their lives,” he says. “A day of high quality could be really important for that person.”
Nazarpour thinks that the technology could be routinely offered to similarly locked-in individuals within the next 10 to 15 years. “For a person that has absolutely no communication, even a “yes”/”no” is potentially life-changing,” he says.
Brian Dickie, director of research development at the Motor Neurone Disease Association in the UK, agrees that this timeline is realistic. But he wonders how many people with motor neuron disease—of which ALS is the most common type—stand to benefit from such BCIs.
Setbacks
The man who received the BCI has a form of ALS called progressive muscular atrophy (PMA). This form of the disease tends to target motor nerves that travel from the spine to muscles, leaving people unable to control their muscles. But around 95% of cases of ALS also involve degeneration of the motor cortex in the brain, too, says Dickie.